If you’re navigating menopause and suddenly dealing with discomfort “down there” or wondering, “Why am I dry down there all of a sudden?”, you’re not alone. Vaginal atrophy, also called genitourinary syndrome of menopause (GSM), is a common condition where vaginal tissues become thinner, drier, and more fragile after estrogen levels drop in midlife. Lower estrogen means less natural lubrication and elasticity in your vagina, which can lead to itching, burning, and pain during sex. That’s the vaginal atrophy menopause connection in a nutshell.
In this article, we discuss the different aspects of vaginal atrophy, exploring its symptoms, causes, impact on intimate relationships, and, most importantly, how you can manage it. Let’s dive in!
What Is Vaginal Atrophy?
Table of Contents
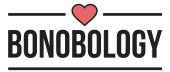
Vaginal atrophy is the thinning and drying of the vaginal walls due to a lack of estrogen. It usually develops during or after menopause, when your body’s estrogen levels fall. Estrogen is the hormone that keeps your vaginal tissue healthy. It helps maintain lubrication, elasticity, and thickness in the vaginal lining. As estrogen dips, the vaginal skin loses moisture and stretchiness. The result? The tissue can become fragile, inflamed, and less able to lubricate itself, leading to some pretty uncomfortable symptoms. Common symptoms of vaginal atrophy include:
- Vaginal dryness and irritation: You might notice a persistent dry feeling inside your vagina or even around the vulva. The lack of moisture can cause itchiness or a raw, irritated sensation
- Burning or stinging: Some women feel a burning sensation in the vagina or when urinating, which is easily mistaken for a urinary tract infection (UTI). In fact, vaginal atrophy can also increase UTI risk due to changes in vaginal pH. Sex during UTI can be immensely discomforting
- Pain during sex (dyspareunia): With less natural lubrication and thinner skin, intercourse can range from uncomfortable to downright painful. Women can also experience minor vaginal tearing or light bleeding during or after sex, due to the fragility of tissues
- Itching inside or around the vagina: Thinning skin can become itchy. Even the vulva can get dry and itchy, so sometimes just putting on underwear can cause irritation
- Frequent urinary issues: Because vaginal and urethral tissues are hormone-sensitive, you might find you have to urinate more often or feel urgency. Some women also experience mild incontinence or recurrent UTIs as part of the genitourinary changes of menopause
Sharing her experience of noticing the vaginal atrophy menopause connection, a woman on Reddit says, “Painful sex was the first atrophy symptom I had. I had never heard of vaginal atrophy and now I don’t shut up about it because I think it’s one of the worst symptoms that I’ve been surprised by.”
It often isn’t talked about openly, so many women feel blindsided when these symptoms hit. If some of these symptoms of vaginal atrophy sound familiar, take heart in the knowledge that this condition is very common and treatable. Up to half of menopausal women experience low estrogen symptoms like dryness and discomfort.
It’s not something you “just have to live with.” There are means to manage these symptoms effectively, and the first step toward making that happen is to understand what’s happening in your body that’s manifesting as all this discomfort. Let’s talk about that.
Related Reading: Five Fulfilling Alternatives To Intercourse
Why Women Experience Vaginal Atrophy During Menopause
So, what are the vaginal atrophy causes, and how does menopause contribute to it? Menopause is typically to blame, due to the hormonal rollercoaster your body goes through. As you approach menopause, your ovaries produce less and less estrogen. This estrogen drop is the main trigger for vaginal atrophy. Think of estrogen as the “maintenance crew” for your vaginal tissues. When it’s in abundant supply during your reproductive years, it keeps the vaginal lining plump, moisturized, and resilient. When that supply shrinks, the vaginal skin starts to dry out, thin down, and lose flexibility, becoming more like delicate paper than elastic tissue.

In fact, low estrogen symptoms often manifest in multiple ways during menopause. You might get hot flashes, night sweats, mood swings, and yes, vaginal dryness is one of those hallmark symptoms of low hormones. The natural acids and fluids that used to keep your vagina lubricated are now in shorter supply, which can also upset the pH balance and protective environment.
This onset can feel sudden for many women, leaving them wondering, “Why am I dry down there all of a sudden?” Explaining why it often feels sudden, Dr. Cynthia Abraham, an OB/GYN, says, “Many patients only realize something is wrong when they attempt intercourse after a period of abstinence and find that sex is painful due to dryness.” So while the tissues may have quietly thinned over time, you notice the dryness only when it starts affecting your intimacy.
How Vaginal Atrophy Impacts Intimate Relationships
The impact of vaginal atrophy menopause connection isn’t limited to your body. It influences your relationship with your partner and can lower self-esteem. As Dr. Abraham says, many women only notice postmenopausal atrophic vaginitis when they experience dryness and discomfort during sex. This can bring up feelings of frustration, lead to a decrease in libido, and even leave you worried about intimacy with your partner.
Painful sex can understandably lead to a decreased sex drive or avoidance of intimacy altogether. After all, if your brain starts to associate sex with pain, it’s hard to feel eager for it. This can create a cycle of both partners withdrawing: you might dread intercourse, and your partner might feel confused or rejected.
Licensed marriage and family therapist Katie Ziskind explains that vaginal dryness can deeply impact a romantic relationship and healthy sex life. “Painful sex is often one of the main symptoms of vaginal dryness,” Ziskind notes, “And that pain can cause anxiety or reluctance around intimacy.”
In turn, couples may experience tension or a loss of closeness. You might find yourself in a pattern of turning down advances or your partner becoming hesitant to initiate, for fear of hurting you. Emotional side effects like feeling “old” or less attractive can creep in as well. A man going through something similar asked for help on Reddit, saying,
“My wife (53) & I (52) have been struggling for the last year with vaginal dryness during sex. It started out with only occasional dryness, which we would work around, but now it’s made penetrative sex nearly impossible because of the pain. I would love to give or get oral sex, but she’s not into it, she says it makes her feel uncomfortable.
“She has hot flashes & hasn’t had her period for about a year. She has gone to the doctor, and Estrogen replacement therapy has been suggested, but at this point, she refuses to start because she has unspecified health concerns. She will not use lube because she gets UTIs & itching from the variety of brands we’ve tried. So I’m here trying to get help for us because I feel that our marriage is at a breaking point, I can not live in a sexless relationship. Please give us advice, what has worked for you?”
It’s plain to see how devastating untreated vaginal atrophy can be for both partners in a relationship. The silver lining is that with openness and the right approach, couples can adapt and overcome these challenges. Here are some things you can try:
- Communication is key. As awkward as it may seem, talking to your partner about what you’re experiencing physically will help them understand it’s not about lack of attraction
- Try to approach it as a team problem to solve, rather than suffer in silence. Often, just validating that “it’s not you, it’s the menopause” can relieve a lot of the emotional strain on both sides.
- Many couples find that working with a sex therapist or counselor can help them navigate these changes. “Couples can gain sex education and sexual confidence from working with a sex therapist,” says Ziskind
- Be open to redefining intimacy. It doesn’t have to mean penetrative sex. Focusing on sensual massages, oral sex (if comfortable), or simply increasing non-sexual affection can maintain connection while you address the physical issues.
- Don’t underestimate the value of patience and humor with your partner. Menopause is a natural phase of life, and while vaginal dryness is serious, it’s okay to approach solutions with a bit of lighthearted teamwork
Vaginal atrophy can affect your sex life, but it doesn’t have to end it. With good communication, the right treatments, and maybe some professional guidance, your sex life can absolutely continue to be satisfying after menopause.

How To Manage Vaginal Atrophy
Ready for the good news? There are many ways to manage vaginal atrophy and relieve that dryness, pain, and irritation. From simple home remedies to doctor-prescribed therapies, you have options. It may take a bit of trial and error to find what works best for your body, but countless women have been in your shoes and found solutions that let them feel comfortable and sexual again.
Before we break these down for you, remember that what works for one woman might not work for another. Your body is unique, so stay open-minded and give yourself some grace and time to find the right regimen. If something isn’t helping or causes new irritation, you can always pivot to another solution. Relief is definitely possible. Here are some solutions to counter the vaginal atrophy menopause connection effectively:
1. Natural supplements for vaginal dryness

One of the first things many women ask is whether there are natural supplements for vaginal dryness—vitamins, herbs, or dietary changes that can boost your body’s lubrication from the inside out. The answer is yes, there are a few promising options,
A 2023 study, along with other studies, for instance suggests that certain vitamins and fatty acids may improve vaginal moisture. Vitamin E and vitamin D have been shown to help increase vaginal lubrication and improve tissue health in postmenopausal women. Similarly, omega-3 fatty acids might support vaginal health by mildly increasing estrogen levels and enhancing lubrication.
Related Reading: Sexual Intimacy: Meaning, Benefits And Ways To Improve
“I’ve tried slippery elm and sea buckthorn oil and both have worked for me,” one Reddit user shared, discussing natural approaches to dryness. “They increase mucus in all mucous membranes. Slippery elm is the most common for vaginal dryness – I would start there first!” Many women in online forums echo that certain supplements helped them “get wet” again or at least improved overall dryness over time. Sounds promising? Here are some natural supplements for vaginal dryness you can explore:
- Membrasin Vitality Pearls (Sea Buckthorn Omega-7): A popular oral supplement rich in omega-7 fatty acids. Membrasin’s formula is designed to restore natural vaginal moisture by nourishing the mucous membranes from within. Some postmenopausal women report less dryness and itching after a couple of months of use
- O Positiv “MENO” Vaginal Moisture Support: An OBGYN-formulated capsule that includes a blend of vitamins like D3 and E, hyaluronic acid, and herbal extracts to support healthy vaginal moisture and tissue comfort. It’s a hormone-free daily supplement created specifically for menopause-related dryness
- OLLY “Mellow Menopause” Capsules: A daily menopause supplement containing EstroG-100, a blend of herbal extracts, along with ingredients to help with mood and stress. EstroG-100 has some clinical backing for menopause symptoms; women say this supplement helped with vaginal dryness, hot flashes, and even occasional mood swings (a nice bonus!)
Of course, maintaining a balanced diet with healthy fats like avocados, nuts, oily fish, and staying well-hydrated can also support your body’s moisture levels. Supplements are not magic bullets, but they can be a helpful part of a holistic approach, especially in combination with direct local treatments, which we’ll discuss next.
2. Estrogen creams and hormonal options
Since vaginal atrophy is fundamentally caused by lack of estrogen, one of the most effective treatments is, unsurprisingly, to add some estrogen back into the vaginal tissue. This doesn’t mean you have to go on full-body hormone replacement therapy (HRT) if you don’t want to. There are low-dose vaginal estrogen therapies that provide targeted relief right where you need it, with minimal absorption into the bloodstream.
Many gynecologists consider vaginal estrogen creams, tablets, or rings the gold standard for moderate to severe vaginal atrophy because they actually address the hormonal deficiency and can even reverse some of the tissue changes over time.
What are the options? There are a few forms of prescription vaginal estrogen that slowly release estrogen:
Related Reading: How to Spice Up A Sexless Relationship and Bring Intimacy Back?
All of these are inserted into the vagina. The ring you leave in place for around 3 months at a time; creams and tablets are used daily or a few times a week. These treatments deliver a micro-dose of estrogen locally, much lower than systemic HRT doses. According to the American College of OB/GYN, they carry very few risks for most women, even those in their 60s and beyond, and the estrogen stays largely in the vaginal tissue. If you have a history of breast cancer or other contraindications to estrogen, you’d need to discuss with your doctor. Often, even cancer survivors can use vaginal estrogen safely.
Women who use vaginal estrogen often report significant improvement in symptoms of vaginal atrophy. It’s not an instant fix; usually you use the product for a few weeks before noticing big changes, and maximum benefits come with regular use over months.
If estrogen cream isn’t an option for you because you absolutely cannot use hormones due to medical reasons, there are other prescription approaches available. One is DHEA vaginal suppositories. DHEA is a hormone precursor that your body locally converts into estrogen and testosterone, helping rejuvenate vaginal tissue. Another is an oral medication called ospemifene, which isn’t estrogen but acts like estrogen in the vaginal tissue to reduce pain with sex. However, these alternatives should be used only when suggested by your doctor.
3. Vaginal moisturizers

When you think of moisturizer, you probably imagine a face or hand cream. Well, your vagina can benefit from moisturizer too! Vaginal moisturizers are OTC products that you apply inside the vagina and sometimes around the vulva on a regular basis, either daily or a few times a week, to hydrate and nourish the tissues.
If you’re dealing with daily dryness or irritation, not just during intercourse, a vaginal moisturizer can be a game-changer. Dr. Cynthia Abraham says, “For vaginal dryness by itself, I recommend trying over-the-counter moisturizers and lubricants as a first line of treatment.”
These products often contain ingredients like hyaluronic acid, vitamin E, glycerin or glycol, and soothing agents. Some are gels or creams you apply with an applicator internally; others are ovule inserts or “beads” that dissolve. Then there are external vulvar moisturizers to relieve itching and dryness around the vaginal opening. Here are some popular vaginal moisturizers you can explore to address vaginal atrophy:
- Replens Long-Lasting Vaginal Moisturizer: A well-known glycerin-based moisturizing gel. It comes with applicators for internal use every 3 days or so. Replens works by coating the vaginal walls and hydrating the tissue; many women feel improved comfort after using it regularly
- Revaree Vaginal Inserts (Hyaluronic Acid): Revaree is a hormone-free vaginal insert made with hyaluronic acid. You insert one vaginal suppository tablet every few days; it dissolves and provides deep hydration. Clinical studies have shown hyaluronic acid can be as effective as estrogen cream for symptoms of vaginal atrophy in some cases, making Revaree a popular new option
- VMagic Organic Vulva Balm: This is an external moisturizing balm with natural ingredients like olive oil, honey, and beeswax that you apply to the vulva to soothe itching, redness, or splitting skin. It’s basically like a gentle, chemical-free lotion for your intimate skin. Women going through menopause love it for daily comfort. It can relieve that dry, sandpapery feeling around the vaginal opening
4. Lubricants for comfortable intimacy
While moisturizers help on a daily basis, you’ll still want a good lubricant on hand for sexual activity. Lubricants are designed to be applied right before intercourse or masturbation to reduce friction and pain. Using lube generously and frequently is one of the simplest and most effective ways to make sex pleasurable again. There are a few types of lubes you can explore:
- Water-based lubricants: These are the most common. They’re compatible with condoms and sex toys, easy to wash off, and generally gentle. The downside is that they can dry out or get absorbed, so you might need to reapply during a long session. If you’re prone to UTIs or yeast infections, look for glycerin-free and paraben-free labels
- Silicone-based lubricants: These are very slick and long-lasting, making them great for people who find water-based lubricants dry up too fast. Silicone lubes are also excellent for use in water because they won’t dissolve. They are safe with condoms, but not with silicone sex toys, as they can degrade the toy’s material
- Oil-based lubricants: This includes natural oils like coconut oil, olive oil, etc., as well as petroleum jelly or mineral oil products. Oil lubricants last a long time and feel moisturizing; however, they’re not compatible with latex condoms and can cause breakages. Some oils can trap bacteria or irritate sensitive tissue with long-term use. Coconut oil is a popular bedroom lubricant for those who don’t need condoms. Many women find it soothing and non-irritating. However, as a rule, doctors often recommend water-based lubes first to avoid any condom or infection issues
Related Reading: 11 Critical Sexless Marriage Effects On Wife
It’s worth trying a few different lubricants to find what texture and formula you like best. Here are some top options from each category you can explore:
- Astroglide Liquid: A classic water-based lubricant that’s been around for ages. Astroglide is known for being super slick initially. It does contain glycerin, which makes it very slippery, but that means some women might need to wash after sex to avoid any irritation. Astroglide is a good basic lube to try. Just reapply as needed since it can get a bit sticky when it dries
- Sliquid H2O or Sliquid Organics Gel: Sliquid is a popular brand formulated specifically for sensitive women. It’s water-based, glycerin-free, and paraben-free, with a short ingredient list. Sliquid H2O is a thin liquid, whereas the Organics Gel is a bit thicker. Both provide cushioning without irritation. Many menopausal women rave that Sliquid doesn’t burn or upset their vaginal pH
- Uberlube Silicone Lubricant: A premium silicone-based lube that comes in a sleek glass pump. Uberlube is extremely silky and long-lasting, with only a couple of ingredient:s silicone and a little vitamin E. It’s great for those who find water-based lubes evaporate too quickly on their tissue. Users often comment that Uberlube feels very natural and even reduces friction for hours

5. Vitamin E suppositories and other home remedies
Now let’s talk about some DIY and home remedies that many women find useful— vitamin E suppositories, coconut oil, and other natural oils. Vitamin E is a star player in this arena. Vitamin E is known for its skin-healing antioxidant properties, and it turns out it can work wonders for vaginal tissue as well. You can find vitamin E vaginal suppositories in the form of capsules or inserts, marketed for vaginal dryness, or you can literally use vitamin E gel capsules from the drugstore.
The idea is to place the capsule in the vagina, usually at night. It dissolves and releases the vitamin E oil, coating the vaginal walls. Women report that this can reduce dryness, itching, and even improve elasticity with regular use. A postmenopausal user shared on Reddit, “Get some cheap vitamin E oil capsules – the gel ones. Pop a couple up the hoo-ha before bed. The gel melts and the oil treats… this was the very best tip I was given.”
She found that vitamin E was more soothing for her vaginal “dry patches” than regular lubricants, essentially acting like a healing salve internally. Many in the thread agreed that vitamin E suppositories or oil provided relief from the “razor blade” feeling of vaginal dryness. You can also purchase pre-made vitamin E suppositories like Carlson Key-E Suppositories, specifically made for vaginal dryness. These are convenient and formulated for easy insertion.
Related Reading: Maintenance Sex—What Is It, Why Is It Important, And How To Have It?
Another beloved remedy is coconut oil. As mentioned earlier, coconut oil can serve as a natural lubricant, but it’s also a day-to-day moisturizer. Some women make little coconut oil suppositories by refrigerating small chunks of extra virgin coconut oil using a suppository mold, then inserting them at bedtime. The oil melts with body heat and coats the vagina. Coconut oil is natural, gentle, and has mild antimicrobial properties, so it generally doesn’t upset the vaginal flora.
Other home remedies people use include olive oil, sweet almond oil, or aloe vera gel applied to the vulva and vagina. These can be soothing for external dryness or mild internal use. Every woman’s chemistry is different, so what feels calming to one person might not agree with another. If you try a natural oil, introduce one at a time and see how you feel. Typically, pure, food-grade oils are safe—just avoid anything with fragrances or additives.
Another option is lidocaine gel. This isn’t exactly a natural remedy, but it’s something some doctors suggest for those with severe pain. A lidocaine gel applied to the vaginal opening 5-10 minutes before sex can numb the area just enough to make initial penetration tolerable while you work on longer-term fixes. It doesn’t take away all sensation, and it can be a useful bridge solution if pain is a big barrier.
Key Pointers
- Vaginal atrophy is a common postmenopausal condition where estrogen loss causes thinning, dryness, and inflammation of vaginal tissues, often leading to painful sex and irritation
- Symptoms include vaginal dryness, burning, itching, painful intercourse, and urinary issues, which can significantly affect quality of life and intimate relationships
- Menopause is the primary trigger, with the drop in estrogen weakening the vaginal lining’s elasticity, moisture, and pH balance
- Treatments include local estrogen therapies, vaginal moisturizers, lubricants, DHEA suppositories, ospemifene, and hormone-free natural supplements like vitamin E, omega-3s, and sea buckthorn oil
- Open communication, therapy, and redefining intimacy are key to managing its emotional and relational impact—it’s treatable, not something to silently endure
Final Thoughts
Dealing with vaginal atrophy during menopause can feel overwhelming, but remember: you have many tools at your disposal. Often, the best approach is a combination of strategies. For instance, you might take a supplement to address internal balance, use a vaginal moisturizer every other day for ongoing hydration, apply a vitamin E suppository or coconut oil as needed, and always use a good lubricant for sex. If symptoms are still troublesome, you can talk to your doctor about adding vaginal estrogen to really get to the root of the issue. There’s no one-size-fits-all, but there is a solution that will work for you.
Your sexual health and comfort matter. Whether it’s using natural supplements for vaginal dryness or asking your doctor about the latest treatments, you deserve to feel good in your body. With the right care routine, those pesky symptoms of vaginal atrophy can be effectively managed. You might even find your confidence and pleasure soaring back once you’ve got everything moisturized and sorted out. Here’s to keeping your lady parts happy and your intimate life thriving through menopause and beyond.
I Have No Sex Drive And My Husband Is Mad: Expert Advises What To Do
Your contribution does not constitute a charitable donation. It will allow Bonobology to continue bringing you new and up-to-date information in our pursuit of helping anyone in the world to learn how to do anything.








Featured
11 Best Supplements for Women’s Libido After Menopause
15 Spectacular Options For Lingerie For Older Women—Classy Yet Sexy
15 Best Lubricants For Menopause Dryness
How To Bring Back Intimacy In A Marriage After Menopause—9 Tips
Painful Sex After Menopause? Try These 9 Time-Tested Solutions
What After Menopause: Understanding How Your Body Changes
10 Best Vibrators for Women Over 50, Rated By Real Women
Menopause and Libido Loss: A Comprehensive Guide for Women
How To Increase Libido After Menopause—9 Easy Ways